Prosthetic Care




Stump care
Massage, Tapping, Desensitisation and Scar Mobilisation.
Desensitisation is believed to reduce pain, help with tolerance and touch in the residual limb and may help the patient with an amputation adjust to his or her new body image that now includes limb loss. Massage and tapping can be started early on and could be done over the soft dressing or when it is off. All these techniques could be done by the therapist and also taught to the patient/family member to do. Also, instruct the patient how to perform desensitization and distraction techniques to reduce the phantom pain.
Massage
- Massage the entire residual limb with 1 or 2 hands by doing soft gentle kneading. Be cautious over the sutured area after scar is totally heal.
- Once the sutures or clips are removed you can increase the pressure on the deeper muscles and soft tissue.
- 5 Minutes 3-4 a day or as needed to reduce phantom limb pain.
- Gently massage the proximal residual limb, to include pressure points in the inguinal region
Tapping (after clearance from surgical team)
- The residual limb should be tapped with fingertips (not the fingernails).
- When the sutures or clips are still in then gentle tapping could be done over the suture line
- This could also be done over the Rigid or soft dressing
- Once the sutures are removed a slapping motion could be done on the residual limb
Desensitisation
- This helps to make the residual limb less sensitive to touch and will improve the tolerance to touch.
- 2-3 times a day when the soft dressing is off (this could be done during or after bathing)
- Start by using a soft material, like a cotton ball, to gently rub the skin in circular motions.
- Progress by using a rougher material, like a paper towel, and then progress to a towel or cloth until you can tolerate these materials.
Scar Mobilisation
- This will keep the scar from adhering to the underlying tissue as it could be the cause of pain and blisters when the patient starts wearing a prosthesis.
- Performed when the soft dressing or compression is off.
- The patient can do this daily when taking a bath
- Place two fingers over a bony portion and by keeping the fingers on the same spot make a circular motion for 1 minute.
- Repeat this over and around the bone on the residual limb
- After wound healing, this could be done over the incision line to mobilise the scar tissue
Stump Skincare
To prevent adhesion of the surgical incision scar on the stump after the surgery, a deep friction massage is performed vertically around the scar line. The prosthesis is worn following stump maturation through desensitization and stump reduction.
Ideal Stump
The ideal stump is one that is well-healed, has a good vascular supply, soft and mobile scars, minimal pain, minimal edema, a length sufficient for biomechanical leverage but not too long to restrict choices for prosthetic components, and large surface areas for distribution of pressure.
Post-operative care – Immediate post-operative prosthesis (IPOP)
The immediate postoperative prosthesis has been purported to allow early functional gain with potential physical and psychological benefits to patients. An IPOP is a complete prosthesis with an upper or lower extremity socket and appropriate components attached.
The IPOP is an application of a rigid cast immediately postoperatively within the operating theatre and attachment of a temporary prosthesis soon thereafter.
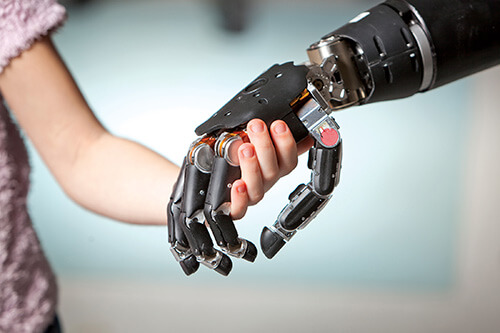
Pre-prosthetic training
Our teams will focus on preparing your residual limb for a prosthesis. This will involve skin care, muscle strengthening, pain management, and limb shaping. Our clinician will guide you toward reaching goals to maximize independence and prepare the limb for prosthetics.
In case of swelling or edema on the stump you have to manage the dynamics of body fluids for which you might have to wear a shrinker or compression sock to control the swelling should be expected. Interventions during the pre-prosthetic training period include therapeutic exercise, range of motion, assistive device training, wheelchair mobility, residual-limb shaping, soft-tissue mobilization, and positioning.

